
Herrera E, Jr Caramelli P, Silveira ASB, Nitrini R. In this sense, dementias are the most prevalent, ranging from 1.6% in elderly people aged 65 years to 38.9% in those aged 85 years and older 3 3. Besides depression, the prevalence of neurodegenerative disorders also increases with aging. Depression morbidity in later life: prevalence and correlates in a developing country. Blay SL, Andreoli SB, Fillenbaum GG, Gastal FL. A study with 7.040 Brazilian elderly people found a prevalence of 22.7% of depressive symptoms 2 2. Prevalence and predictors of depression in populations of elderly: a review. The prevalence of major depression in the elderly people ranges from 0.9% to 9.4% in private households 1 1. Além disso, a idade, o nível educacional e a capacidade cognitiva são variáveis que podem influenciar o desempenho na avaliação objetiva.Įnvelhecimento saúde mental aptidão físicaĭuring the aging process, there is an increase in the prevalence and incidence of mental disorders, such as depression and dementia. ConclusõesĪpesar de a menor aptidão cardiorrespiratória de idosos com DM e DA ter sido encontrada nas duas avaliações, os resultados devem ser observados com cautela, uma vez que os testes apresentaram baixa correlação e classificações de risco de perda funcional divergentes. DA também não mostrou diferenças no STEP em comparação aos saudáveis, quando controlado pelo MEEM (p = 0,261). Controlado por idade e escolaridade, não houve diferenças entre os grupos no Step (DM, p = 0,097 DA, p = 0,102). ResultadosĭM e DA apresentaram menores escores comparados aos saudáveis no nomograma VSAQ (p < 0,001) e no teste Step (p = 0,009 e p = 0,008).
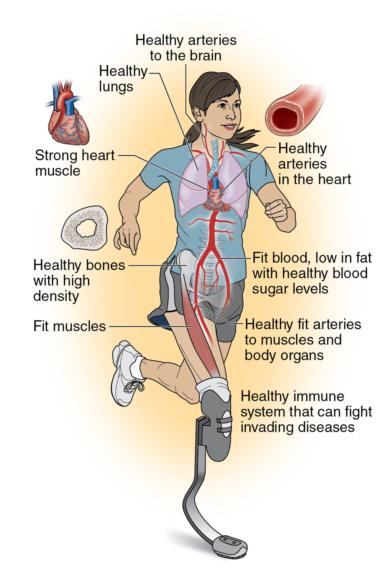
Os sujeitos responderam a escala de Hamilton (HAM-D), Miniexame do Estado Mental (MEEM), VSAQ (Veterans Specific Activity Questionnaire) e o teste 2-minute Step. MétodosĬinquenta e sete idosos (72 ± 7,9 anos) foram divididos em três grupos: DM (n = 20), DA (n = 17) e saudáveis (n = 20). In addition, age, level educational and cognitive performance are variables that can influence the performance objective evaluation.Īvaliar a capacidade cardiorrespiratória em idosos com depressão maior (DM), doença de Alzheimer (DA) e saudáveis, subjetiva (nomograma VSAQ) e objetivamente (2-minute STEP). Conclusionsĭespite the lower cardiorespiratory fitness of elderly patients with DM and DA have been found in both evaluations, the results should be viewed with caution, since the tests showed low correlation and different risk classifications of functional loss. AD group did not present differences to healthy group for Step, when adjusting for MMSE (p = 0.261). Adjusted for age and educational level, no differences among groups were observed for Step (MDD, p = 0.097 AD, p = 0.102). MDD and AD showed lower scores than healthy group for Nomogram VSAQ (p < 0.001) and 2-minute Step (p = 0.009 p = 0.008, respectively). The subjects answered Hamilton Scale (HAM-D), Mini-Mental State Examination (MMSE), Veterans Specific Activity Questionnaire (VSAQ) and 2-minute Step test. Methodsįifty seven subjects (72 ± 7.9 years) were divided into three groups: MDD (n = 20), AD (n = 17) and Healthy (n = 20). These opportunities must be realized to optimize the prevention and treatment of cardiovascular disease and hence meet the American Heart Association's 2020 goals.ĪHA Scientific Statements cardiovascular disease physical fitness risk factors.To assess cardiorespiratory capacity through subjective and objective tests in older adults diagnosed with major depression (MDD), Alzheimer disease (AD) and healthy older adults. The underlying premise of this statement is that the addition of CRF for risk classification presents health professionals with unique opportunities to improve patient management and to encourage lifestyle-based strategies designed to reduce cardiovascular risk. Although the statement is not intended to be a comprehensive review, critical references that address important advances in the field are highlighted. The purpose of this statement is to review current knowledge related to the association between CRF and health outcomes, increase awareness of the added value of CRF to improve risk prediction, and suggest future directions in research.
A growing body of epidemiological and clinical evidence demonstrates not only that CRF is a potentially stronger predictor of mortality than established risk factors such as smoking, hypertension, high cholesterol, and type 2 diabetes mellitus, but that the addition of CRF to traditional risk factors significantly improves the reclassification of risk for adverse outcomes. Mounting evidence has firmly established that low levels of cardiorespiratory fitness (CRF) are associated with a high risk of cardiovascular disease, all-cause mortality, and mortality rates attributable to various cancers.


 0 kommentar(er)
0 kommentar(er)
